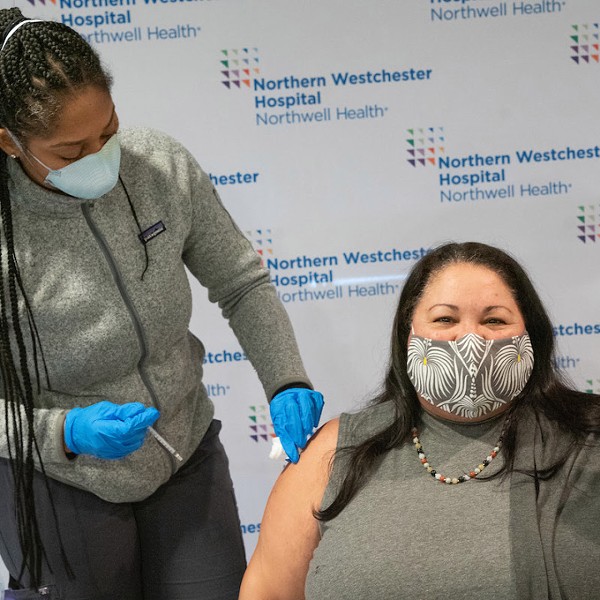
State by state, America is reopening after sheltering in place and we're doing it on a wing and a prayer—or at least, with a face mask and rubber gloves. Only a few protections stand between us and a virus so menacing, it actually has spikes. Even more than disinfectant wipes and hand washing, we need good science to fight COVID-19.
A safe, widely available vaccine could take months to roll out, as cells in a petri dish can only grow so fast. That's why scientists are carrying out parallel efforts to explore more rapid-fire solutions. Around the globe and close to home, doctors and researchers are uncovering every stone—from repurposing existing drugs to developing antibody treatments and exploring nutraceuticals that could offer safe, affordable protection naturally. The following two research endeavors hold promise, and they're unfolding right here in our local communities.
Finding Hope in Glutathione
When his 48-year-old mother struggled to recover from COVID-19 in late March, James Bruzzese, a second-year medical student at CUNY School of Medicine in Harlem, knew where to turn. He called his mentor, Dr. Richard Horowitz, a board-certified internist with a private integrative medicine practice in Hyde Park. Considered among the country's top Lyme disease doctors, Horowitz has built a practice around combining classical and complementary treatments for tick-borne infections. Not everyone jibes with Horowitz's style—some online patient reviews bristle with talk of long waitlists and steep à la carte expenses for his services. But after he became instrumental in helping Bruzzese's younger sister, Julia, in her battle with Lyme, Bruzzese grew close to the doctor. "He's been letting me shadow him, so every time I get a little break from school, I do that," says the 23-year-old Brooklynite. "I've been exposed to a lot in his practice and it's been an amazing experience."
Bruzzese's mother, Josephine, had woken up on the morning of March 22 with severe symptoms in line with COVID-19—fever, body aches, coughing, and such severe shortness of breath that she couldn't get up from bed. "It was scary from the start," recalls her son. His family called New York's coronavirus hotline, which advised getting her to an emergency room. When her ambulance pulled in at NYU Langone Hospital in Sunset Park, Brooklyn, the ER was eerily empty. The hospital had no coronavirus tests at the time, but a lung X-ray showed that Josephine had severe lobe pneumonia and she was clinically (if not serologically) diagnosed with COVID-19 on the spot. Yet the doctors declined to admit her—instead, they gave her a dose of Zithromax (azithromycin) and sent her home with four more days of the oral antibiotic. Bruzzese was shocked. "We learn as medical students that the treatment for pneumonia is IV antibiotics," he says. "They didn't even do a culture. On my board exams, if I were to answer a question about a patient presenting with pneumonia and I didn't say, 'Order a culture to see what type of bacteria it is and [administer] IV antibiotics,' I would get that question wrong. What was going on during this crisis, just giving people a very weak oral antibiotic for a severe pneumonia, was just crazy."
Bruzzese knew his mother needed more. Back home, the family happened to have Plaquenil (hydroxychloroquine) on hand because of his sister, but they didn't want to administer it blindly. He reached out to a local doctor for guidance who advised him on dosing, and Josephine remained on Zithromax and Plaquenil for about 10 days. Her fever and body aches went away, but the respiratory symptoms lingered. "She was still coughing like crazy and couldn't breathe," Bruzzese recalls. That's what prompted him to reach out to Horowitz for help. "I called him in desperation, and I gave him the rundown like I would do on rounds." (Current FDA guidelines caution against the use of hydroxychloroquine for COVID-19 treatment outside of the hospital setting.)
As it turned out, Horowitz had recently treated another COVID-19 patient successfully with a simple, natural therapy—glutathione. Produced in the liver and also available to take as a nutritional supplement, glutathione is one of the body's main antioxidants. It assists with detoxification and helps to combat free radicals, the molecules that can damage cells when there is too much inflammation in the body. "He said, 'If you're willing, let's see if it helps your mom, too,'" recalls Bruzzese, who happened to have glutathione in the family medicine cabinet. Horowitz suggested a 2,000-milligram dose, and within an hour Josephine was breathing easier and even got out of bed to take a shower. The next morning, she took a double dose and felt even better, and in the following days she made a full recovery. "We saw these miraculous effects very quickly," says Bruzzese, "and Dr. Horowitz said, 'We need to write this up. This is definitely something.'" With Bruzzese as a coauthor, Horowitz went on to publish a study of the two patients in the online journal Respiratory Medicine Case Reports in May.
"It is a miracle and it's not," says Horowitz of glutathione, which he has used on thousands of patients in his medical practice over the past 30 years. "It's already in the literature—there are published articles on glutathione showing that it has anti-viral activity against herpes viruses, HIV, and hepatitis. The problem is, all of the COVID research is happening through pharmaceutical companies. No one is looking at natural approaches. You hear a little about how low vitamin D might put you at risk, so it's coming out in dribs and drabs." And just like with vitamin D, you can be deficient in glutathione—especially if you've been exposed to a lot of environmental toxins (which is everyone). Older people are also more likely to be depleted of the compound.
Horowitz's a-ha moment with glutathione came from reading dozens of scientific articles about COVID-19. "I saw that the inflammatory molecules that are released when people are exposed to COVID are exactly the same inflammatory molecules that are released when you're exposed to Lyme," he says. "There's a cytokine storm that happens, which is like a fire in the body, a huge inflammatory reaction that can affect all the organs. And we know that with COVID, it's not the virus itself that's killing people. It's this overstimulated immune response with all the inflammation. When I saw that the cytokines in COVID were the same molecules in Lyme, I thought, well, we already know how to lower these cytokines." (Cytokines are molecular messengers between cells. Inflammatory cytokines are molecular messengers that can increase the inflammatory response.)
On a biochemical level, the way to reduce this inflammation is to turn off a switch inside the nucleus of the cells called NF-kappa-B. Three different compounds effectively shut down these inflammatory cytokines: glutathione itself; N-acetylcysteine (NAC), which is the precursor of glutathione; and alpha lipoic acid, which helps to regenerate glutathione. Horowitz recommends taking all three as supplements—600 mg of NAC two to three times a day; 600 mg of alpha lipoic acid once or twice a day (the higher dose can cause reactive hypoglycemia in sensitive individuals); and 250 to 500 mg of glutathione twice a day—as a preventive measure against COVID-19. People who have multiple chemical sensitivities or a sulfa allergy should be careful using glutathione, as it could cause an allergic reaction (Dr. Horowitz has seen this only rarely in IV forms of glutathione). The oral version is generally safe for everyone, but it is always best to check with your healthcare provider before starting a new regimen.
The next step is to conduct a randomized controlled study of glutathione for COVID-19, but Horowitz will need help to make that happen. One way would be to give the therapy to residents at a nursing home at high risk and see how well it protects them compared to residents of a nursing home that doesn't use it. He reached out about a glutathione study to his contacts in government after serving on a committee that gave recommendations on tick-borne diseases to Congress—and got back only two responses. "The medical journals are excited about remdesivir, an antiviral that only lowers your course in the hospital by four days," he says. "I'm sorry, but we're not going to base our hopes on getting four days less in the hospital. We really need something that's going to protect the public now, that is cheap, safe, and effective. Based on the peer-reviewed literature, and my clinical experience, there is a high likelihood that it will be NAC, alpha lipoic acid, and glutathione."
The upshot: The evidence on glutathione for COVID-19 is anecdotal and we need a solid study to explore its potential.
An Arsenal of Antibodies
If anyone knows the importance of controlled clinical trials, it's the folks at Regeneron, a local biotech company that has seven FDA-approved medicines and about 20 investigational drugs in the pipeline. Headquartered in Tarrytown, with manufacturing facilities near Albany and in Ireland, Regeneron is buzzing with COVID-19-related activity these days. "This is a once-in-a-career thing for many people," says Alexandra Bowie, Regeneron's senior director of corporate communications, about her colleagues' opportunity to help find a cure for the biggest health crisis of our time. "The company has really rallied around this and made it our main priority, while still ensuring that we're able to deliver the medicines we make and give to people every day. We're shifting a lot of our R&D resources, our clinical resources, to prioritize the COVID projects." While the endgame is to develop a vaccine, that's not in Regeneron's wheelhouse, but they are going full force on two projects that harness their expertise. One looks to repurpose an existing medication—the FDA-approved rheumatoid arthritis drug Kevzara—while the other is a novel antibody therapy that could serve as a bridge of protection before a vaccine is widely available.
Jointly developed by Regeneron and the French pharmaceutical firm Sanofi, Kevzara (sarilumab) is an injectable medication that inhibits the pathway of an inflammatory cytokine called interleukin-6 (IL-6). "Some data came out of China indicating that IL-6 medicines may be helpful in addressing some of the [hyperactive] inflammatory response that comes at late stages of COVID-19," says Bowie. However, that data came from a 21-patient trial without a placebo group for comparison. So, Regeneron and Sanofi quickly launched a larger, double-blind trial to investigate the drug further. The results from phase 2 of the trial, which was conducted in both severe and critical hospitalized COVID-19 patients, did not show much effect on the severe patients—though it did show a positive trend in the critical patients at high doses. The next step will be to focus only on critical patients in phase 3 of the trial. "We'll see what goes on there," says Bowie, "but this really confirms how important it is to conduct trials with rigor, and with a placebo arm."

Regeneron is more optimistic about its work creating a novel antibody treatment for COVID-19. The idea is that if you can find an antibody, or combination of antibodies, that can block the spike protein on the SARS-CoV-2 virus (coronavirus) cell, then you are effectively disarming it, because the virus uses its spikes to infect into healthy cells. To find these virus-neutralizing antibodies, Regeneron uses its VelociSuite platform, which is an antibody discovery development technology. "Essentially, we've replaced portions of a mouse's immune system with a human immune system, with genes that code for human immune response," explains Bowie. "When these mice are challenged with a virus or a bacteria, they produce antibodies, which are protective proteins, that look just like human antibodies. We then comb through those antibodies and pick the ones that are the most potent at blocking the virus." (If this sounds very Frankenstein, it is, especially to anyone interested in animal rights. Unfortunately, the FDA requires animal testing for most new medicines, though Regeneron says it adheres closely to the industry's ethical laws related to animal welfare.)
Moving quickly, Regeneron has already created a cocktail of two antibodies, and the treatment will go into clinical trials in humans in June. They chalk up their speed to their prior experience developing similar antibody cocktail treatments against Ebola as well as against Middle Eastern Respiratory Syndrome (MERS), which is another type of coronavirus.
It's important to note that an antibody treatment differs from a vaccine in a number of ways. While a vaccine "teaches" the body how to make antibodies that protect against a pathogen, an antibody treatment skips that step and simply administers the necessary antibodies directly into people. Unlike a vaccine, which can protect you for years or even a lifetime, an antibody treatment is effective for only a month or so. But it could offer stop-gap protection, especially for high-risk groups like healthcare providers, who could be re-dosed as needed. More important, an antibody treatment could also help treat people who are already infected, effectively curing the virus. "That's why we think that our option is really a bridge to a vaccine," says Bowie. "We're still going to need a vaccine in the longer term, but this can be a good solution for the next year or however long we need it."
The upshot: Kevzara might help treat critical COVID-19 patients, but Regeneron's antibody treatment is the one to watch as we await results from the clinical trials. Stay tuned.