Leroy Pryce was born 33 years ago at the former Benedictine Hospital on Mary’s Avenue in Kingston, where his mom was a nurse. Watching the way she cared for other people inspired him to pursue a career in health care. In 2012, Pryce began working as a tech at Kingston Hospital, on Broadway, which had merged with Benedictine as part of HealthAlliance of the Hudson Valley. He worked evening shifts while attending nursing school during the day, eventually becoming a registered nurse at the hospital. “I felt a lot of loyalty because I grew up in this town,” he says.
Pryce loved the work, but the long hours and rough shifts began to take a toll. After Westchester Medical Center Health Network (WMCHealth) purchased HealthAlliance in 2016, the culture started to change. Decisions to cut costs and consolidate services made it “more and more apparent, as time went on, that we were no longer that little community hospital,” he says.
Then COVID hit, and Pryce’s relationship to the hospital really deteriorated. A devout Muslim, he had a long beard, and N95 masks didn’t fit his face properly. HealthAlliance couldn’t reliably supply him with a powered air-purifying respirator, a hooded device often used as an alternative to N95s for employees with facial hair, so he was given a choice: go on unpaid leave, or shave the beard. Pryce and his girlfriend were planning to buy a house, and he didn’t want to be the reason they couldn’t. So he cut off his beard.
What bothered him was not being forced into a choice, but the manner in which it was communicated. “The way an entity can treat you, when it’s not someone who loves and cares for you—there was a profound lack of compassion,” Pryce says. He started to see his job differently. Then last fall, he got recruited by Travel Nurse Across America, a healthcare staffing firm based in Arkansas that places nurses at hospitals on a temporary, as-needed basis. Pryce had seen several friends leave staff positions to become travelers, and the gig offered a lot of perks, including weekly paychecks nearly twice as high as the biweekly checks he was bringing home from HealthAlliance.
“With all the stuff that was going on, I was like, ‘Why am I going through this here?’” Pryce says. “??It doesn’t pay for them to be loyal to us, and I don’t think it necessarily pays for us to be loyal to them.” Last October, he made the leap to travel nursing with TNAA, and signed his first contract with Garnet Health Medical Center in Middletown.
Beating Burnout
During the pandemic, two emergencies have unfolded inside hospitals across America. One is the suffering of patients; sometime in early May, the US will exceed one million confirmed COVID deaths. The other is the wellbeing and working conditions of the nurses who care for them.
Bedside nursing is hard. Twelve-hour shifts are routine—as is coming in early, or on your day off, or staying late. The work is physically and emotionally demanding, and burnout is common: a 2019 report from the ??National Academies of Sciences, Engineering, and Medicine found alarmingly high rates of burnout that were damaging to quality of care and harmful to healthcare workers. It called for a systemic overhaul “to address burnout that focuses on the structure, organization, and culture of healthcare.”
COVID only made things worse, overtaxing a system that for decades has attempted to maintain a tenuous equilibrium that precisely matches the number of nurses to the number of occupied beds. Repeated surges have overrun the capacity of many hospitals, traumatizing front-line healthcare providers in the process. A survey of acute and critical-care nurses last September found that 66 percent have considered leaving the profession because of experiences during the pandemic. Nearly 1 in 5 healthcare workers have quit their jobs over the past two years.
Some have become travel nurses. Even before COVID, travel nursing was a growing industry, offering gig-economy flexibility and an escape route for nurses who felt stuck. Between 2009 and 2019, revenue in the sector tripled, according to data from Staffing Industry Analysts. But COVID turbocharged that growth, and it hasn’t slowed even as caseloads have lightened. Hospitals that needed emergency infusions of nurses early in the pandemic are now dealing with staffing shortages as nurses quit in droves. Travel nursing is now the leading driver of healthcare staffing revenue, and is projected to grow another 40 percent this year.
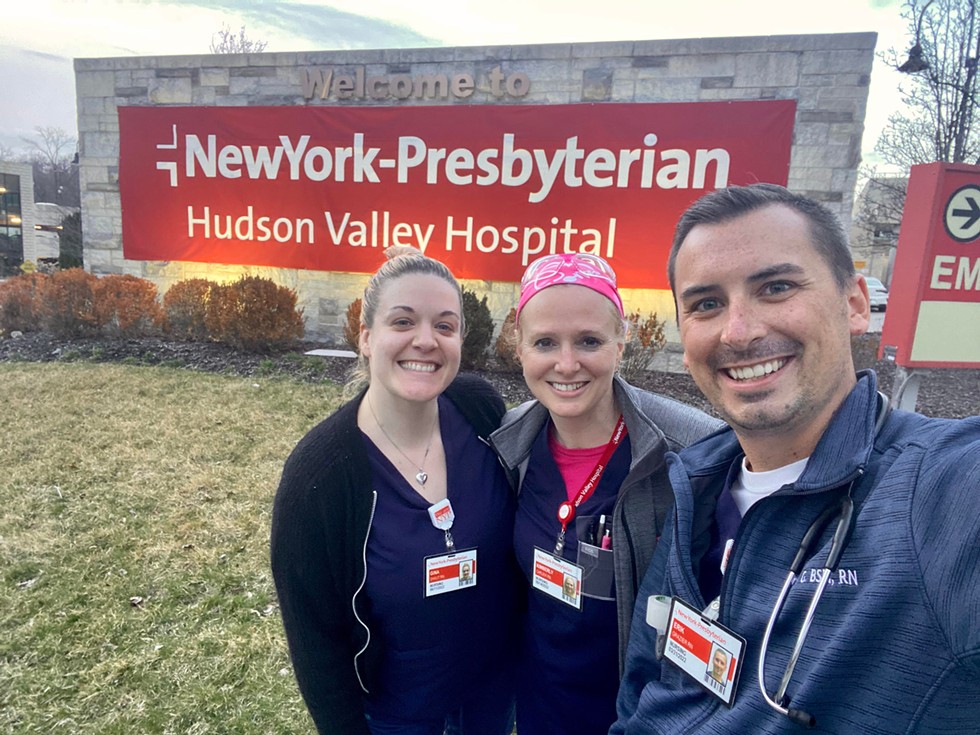
Erik Grazier is one nurse who left a staff job to become a traveler. Like Pryce, he had a long work history at HealthAlliance of the Hudson Valley: first as a tech, then as an ER nurse, and then in the Broadway campus’s new cardiac catheterization lab. But he had grown unhappy at the hospital, and was seeing more and more advertisements for travel jobs on Facebook. Last September he left HealthAlliance and signed on with American Mobile, one of the country’s largest travel-nursing agencies, which connects healthcare professionals with opportunities via an app. Grazier filled out a profile with his background and specialties, and browsed through a list of openings filtered by location, pay rate, and shift. He eventually chose another hospital in the region: NewYork-Presbyterian Hudson Valley Hospital in Cortlandt Manor.
Leaving was a “super easy decision,” Grazier says, in part because “the money that was being offered was almost too good to be true.” Not only was his new pay rate much higher, but like many travel-nursing agencies, American Mobile offers a healthy, tax-free stipend covering transportation, food, incidentals, and even housing for nurses whose primary residence is more than 51 miles from the hospital they sign with. Grazier has been able to pocket some of the stipend. His overall income has tripled.
Grazier’s story is not unique. In April 2020, during the early COVID-19 surges, national wages for travel nurses rose 25 percent. Travel nurses now can be paid anywhere between $3,500 and $10,000 per week. Compare that to staff nurses at hospitals, who in 2020 earned a median salary of $75,330 per year, or approximately $1,450 per week.
That level of pay may not be sustainable in the long run—many travel-nursing agencies have boosted salaries with the help of federal pandemic stimulus funds, and the American Hospital Association is pushing for a congressional inquiry into their pricing practices. Several states are also considering legislation to cap pay for travel nurses. But Grazier says he went into traveling “knowing that what I’m making now will definitely not be forever.” Pryce sees travel nursing as a temporary, financially motivated move enabled by his relative youth, able-bodiedness, and living situation. “If you can bear down and do this for a year, maybe two, and really save money—like, I’m gonna get debt-free,” he says. “I’m going to put aside a little nest egg. Ten years down the line, I may be looking back at this and being like, ‘I’m so, so happy I did that.’”
Why Stay?
Travel nursing is not without drawbacks. Chief among them is a lack of stability: travelers lack the robust union protections staff nurses have, and generally work on contracts ranging from four to 13 weeks. If the hospital still has a need, it may extend the contract, but work agreements can also be terminated at any time. What looks like job flexibility to one nurse looks like precarity to another.
Travel nurses also have little say over their schedules, get no paid time off, and sometimes are given less desirable assignments. More travel agencies are offering health insurance, but that’s by no means a guarantee in the field. And almost by definition, the work is more stressful. Travelers are sent where there is the most need, which means high-risk environments with heavy volume and acuity. During the worst of the pandemic, these were often the places that had PPE shortages and overwhelming COVID surges.
There’s also the challenge of constantly having to acclimate to new surroundings and learn new processes. “You almost never walk in comfortable,” Pryce says. “Which isn’t to say you don’t get comfortable, because you do. But coming from a job where I knew a bunch of people on every unit for every shift, the adjustment can be hard.” On his first day at Garnet, he recalls noticing that the hospital used different needles and a different IV start kit than what he was used to. “I’m not an anxious person, but I had so much anxiety regarding my job for the first time in years, and it was so weird. It was embarrassing.”
The lack of consistency can also be lonely. Catskill native Vanessa Holzmann has been traveling since 2014. A paramedic and trauma nurse by training, she started traveling in order to see new places. Her first assignment took her to Eugene, Oregon, where she knew exactly zero people. “You’re really out of touch with any of your support,” she says. “And we see a lot of terrible stuff. We go through psychological trauma daily, especially ICU nurses. Friends and family are a phone call away, but it’s not the same as being in person.”

Lawrence Clayton, a nurse at HealthAlliance Hospital: Broadway Campus, says he gets multiple phone calls and texts every day from traveling nurse agencies promising big bucks to go elsewhere. “Why do I stay? I have a young child here,” he says. “And I feel responsibility to my colleagues and my community.”
“If They Paid Us What We’re Worth…”
Any work environment travel nurses enter is fraught with potential tension. Travelers are often making much more money than staff nurses, but don’t have seniority, and may lack specific, local expertise, whether in the community of patients or with basic hospital protocols. That can lead to resentment from staff, though the travel nurses I spoke with for this article all say they haven’t experienced that situation—at least during the pandemic, when hospitals have been thankful for whatever help they can get.
And for some, there are benefits to this lifestyle. Grazier has picked up new skills due to working in a wider variety of units than he had access to as a staff nurse. Holzmann is an extrovert, and her ability to make friends easily—plus the fact that she began seeing some fellow travelers across multiple gigs—eventually mollified her loneliness. It has also given her new insight on the profession. “Being a traveler, I see the vast differences between working in different healthcare systems and in different locations,” she says.
Holzmann enjoys working in California, the only state in the US to mandate nurse-to-patient ratios for all specialties (New York has tried, and failed, to implement its own staffing law). “Reasonable ratios are the safest thing we can do for patients and for staff,” she says. Her plan is to stop traveling next year and pursue flight nursing. She’ll be paid less than if she were a hospital staff nurse, but the money she’s saved as a traveler will allow her to pursue a career path she has long deferred. Plus, she says, “life’s not all about, you know, making money.”
Nevertheless, local hospitals are offering more incentives, including higher pay, to retain staff. Grazier says WMCHealth gave out a $10,000 bonus last year for workers who renewed their contracts. William Van Slyke, a spokesperson for Columbia Memorial Hospital in Hudson, says “as with most industries today, staffing for healthcare can be challenging.” He touts CMH’s “competitive rates of pay, comprehensive benefit packages, flexible schedules, retirement plans, tuition reimbursement, and positive and compassionate work atmosphere.”
But for nurses like Grazier, these actions are too little too late, especially in an industry that has systematically undervalued and overburdened its workers. “If they had paid nurses what we’re worth and what we deserve, then the majority of the nurses who jumped ship during this pandemic probably wouldn’t have,” he says.
Plus, he adds, “I was really burned out at Kingston, and was actually looking into changing my career. Travel nursing deterred me from that. I found my passion again.”
This article was also published in the May 2022 issue of Chronogram.