COVID-19, a virus that jumped from bats to humans, has been a sobering lesson in how destructive diseases can be when newly introduced from an animal to a human host. But a plethora of previously existing emerging diseases continue to worry scientists.
The Hudson Valley is home to many research projects on disease ecology and the transmission of emerging diseases from animals to humans. In particular, the area is a focus for scientists who study “vector-borne” diseases: those that are spread between humans, or from animals to humans, through a “vector” species such as ticks or mosquitoes.
The devastation wrought by the pandemic has only made it more clear that the study and surveillance of diseases from the natural world is vitally important if we hope to predict or prevent the next pandemic. But according to some local experts, the intense focus on COVID has distracted public and private health systems from the threat of existing vector-borne diseases in the region.
Local examples include familiar illnesses like Lyme disease and West Nile virus, but also newer or less common pathogens like ehrlichiosis, Powassan virus, and Eastern equine encephalitis. Fueled by a warming climate and changes in human behavior and development, these illnesses are growing in geographic distribution and caseload, harbingers of potentially more severe epidemics in the future.
Ticks
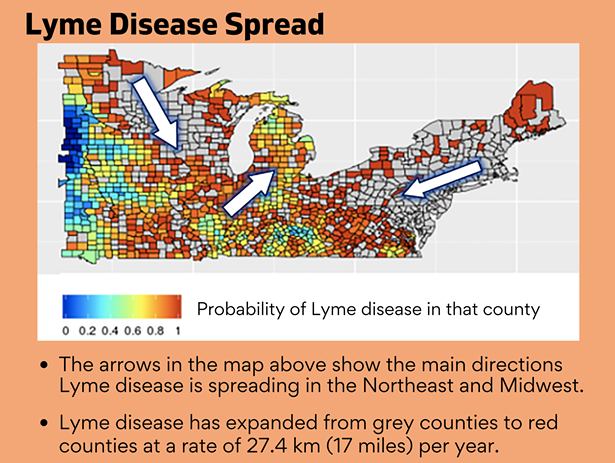
“Ticks have been the story for the last several years, in that the spatial range of where people are getting tick-borne diseases has been changing, and the instance rate—the numbers of people getting tick-borne diseases—has been growing,” says Dr. Shannon LaDeau, disease ecologist at Millbrook’s Cary Institute. Lyme disease, which was first identified in the 1970s (though it presumably existed far earlier), now infects almost half a million people per year, according to the CDC. Cases are concentrated in the Northeast, and within New York State, the Hudson Valley is a Lyme hotspot.
But Lyme disease is not the only tick-borne illness regional scientists worry about. The blacklegged (or deer) tick, which transmits Lyme, can also carry babesiosis, anaplasmosis, ehrlichiosis, and Powassan virus, according to the New York State Department of Health. “The numbers of pathogens we’re seeing people become infected with are increasing,” says LaDeau. “[We are seeing] co-infection where people are also infected with babesiosa, which is a protozoa, or ehrlichiosis, which is a bacterial pathogen, creating real problems.”

Dr. Maria Diuk-Wasser, professor of ecology at Columbia University, says that other tick varieties are spreading across the Northeast. The lone star tick, a common species in the southeastern US whose range is expanding northward, can carry ehrlichiosis and sometimes produces “alpha-gal syndrome,” a meat allergy, in individuals it bites. The Asian longhorned tick, first found in the US in 2017, is also being monitored closely as a potential human disease vector.
Mosquitoes
Due to its harsh winters, the Northeast historically has not had to contend with mosquito-borne illness to the same degree as warmer parts of the country. As LaDeau explains, “the length and coldness of winter are both very strong filters on any pathogen building up in mosquito populations.”
This may be changing. One reason is urbanization. Cities experience a “heat island” effect, producing consistently warmer temperatures due to population density, infrastructure, building materials, and a lack of greenery, which can allow mosquito populations to more effectively survive over winter. But according to LaDeau, cities also provide sites for unique cross-species connections. Urbanized environments bring a variety of species together—birds, mosquitoes, small mammals, humans, and other organisms—that would not naturally come into contact.
Consider a backyard bird feeder, LaDeau says, located near stagnant water that is a breeding habitat for mosquitoes. Such a setup produces “novel interactions between mosquitoes and birds that wouldn’t otherwise happen, or between two different species of birds that wouldn’t otherwise happen”—a process dependent upon human-built environments, and a more likely transmission environment for illnesses.
Two mosquito-based pathogens stand out as particular concerns: West Nile virus and Eastern equine encephalitis. Both have existed in the Northeast for a long time: EEE’s identification dates back to the 1800s, while West Nile first appeared in the United States about two decades ago. Both are also fairly rare, at least in severe cases, but as LaDeau explains, a lot is unclear due to a lack of testing. If mosquito populations rise, the risk of West Nile and EEE should also rise. “It’s fair to assume that if you have more of those vectors, you will have a higher risk of human disease outbreak,” she says. “But that’s a pretty coarse target,” and does not consistently explain the reality on the ground.
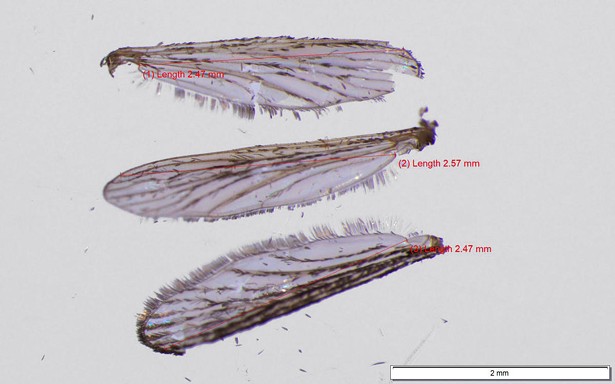
Recently introduced mosquito species, like their tick counterparts, are also a problem. LaDeau points to the tiger mosquito (Aedes albopictus) as a particular threat: “[It is] fundamentally changing the kind of urban mosquito communities in New York City and south, and has been more limited in its establishment farther north, but is increasingly building up populations,” she says. The tiger mosquito is a “very aggressive daytime biter,” and in other parts of the world, acts as a vector of dengue virus and chikungunya virus. As the species becomes more established, it may allow diseases previously unknown in the Northeast to flourish. “Obviously, we don’t have outbreaks of those things here,” LaDeau says. “But that is predominantly because we don’t have large populations of that vector here.”
The Complexity of Expansion
Scientists who study the spread of diseases from wildlife to humans agree that it is becoming more of a problem, but their understanding of the expansion process is still limited. “It is really difficult to identify a single factor responsible for the increases in vector-borne diseases that we are seeing,” says Dr. Laura Harrington, director of the CDC Northeast Regional Center for Excellence in Vector-Borne Diseases.
Harrington recognizes a combination of factors, including climate change, range expansion, globalization, and inadequate education and public health messaging. The spaces where these variables intersect pose the greatest challenges for scientists and contemporary modeling—and prevention—efforts.
Diuk-Wasser points to the reforestation of the Northeast over the last century, coupled with increased suburbanization of areas where deer and other animal populations roam widely, as creating a “perfect storm” for spread of tick-borne diseases. But even this fails to fully capture at the micro level where and why spread is increasing—and what is to be done about it. LaDeau notes the difficulty of “trying to capture both the human behavior and built infrastructure components, and the interactions with climate,” to effectively understand limits on vector and pathogen spread.
For instance, she describes an experiment where her team warmed the soil where blacklegged ticks were overwintering, and found that while the ticks seemed to survive cold temperatures well, warmer soil allowed them to survive even more effectively.
Harrington, for her part, has been studying nuances of the little-understood mosquito mating system. “Recent findings in this area include the discovery that males and females sing to each other (communicate acoustically) prior to mating, and this step is important for reproduction,” she says. “We’ve also learned that male mosquitoes transfer a suite of proteins in their semen during mating that influence females in important ways,” including increasing her blood feeding appetite, ability to lay eggs, and to survive.
Gaps in the Research Landscape
All three scientists point to significant gaps in the contemporary research landscape. “I worry that we don’t have the collaboration among research groups that leads to innovation,” writes Harrington. “Vector-borne diseases are just one of our concerns federally, even when we just look at infectious diseases, and this means that vector-borne diseases receive a minuscule slice of the funding allocation pie.”
Diuk-Wasser concurs. “I think proportionally there’s very little research, compared to the toll it has on people. And it’s not just the disease itself. People don’t use the outdoors, because they’re overwhelmed by ticks, affecting lifestyle and health in many different ways.”
For LaDeau, the problem is in some sense one of precedence. “It is hard to prioritize this research over some other types of public health threats that are always bigger threats,” she says. “The time to address vector-borne disease is before the vectors get abundant, but the willingness to address them or the urgency doesn’t tend to happen until after disease outbreaks are occurring.”
COVID-19, perhaps unsurprisingly, is a part of this research shortfall. LaDeau describes how the immediate and potentially severe risk of COVID displaced other health concerns. Harrington points to specific research gaps that opened over the last year. “The outbreak shifted focus away from vector-borne diseases, understandably, because public health staff were needed to deal with the outbreak,” she says. “We definitely noticed an impact on the ability of health departments to conduct surveillance. Many units completely abandoned their vector-borne disease monitoring and education activities, despite the fact that people were still getting exposed and sickened from vector-borne diseases.”
This is troubling, given that regional vector-borne diseases resulted from the same process as COVID-19: from pathogens that leapt from nonhuman species to humans. “All of the vector-borne diseases we know of affecting humans, including dengue and malaria and things that don’t require that zoonotic reservoir anymore, originated as zoonotic diseases,” says LaDeau. “I do think that there should be more public recognition of what that means now.”
Prognosis and Prevention
The scientists readily concede that the future spread of existing vector-borne diseases—and potentially new ones—is concerning. Both Diuk-Wasser and LaDeau say that increased spread north, to a point, is a major regional expectation for both ticks and mosquitoes, along with corresponding disease spread.
While this appears to be due in part to climate change, modeling even around rising heat is deceptively complex. Ticks are very sensitive to desiccation; mosquito populations can also decrease in intense summer heat, as water for breeding grounds dries up. Climatic factors also intersect with particular urban and suburban factors, as well as human behavior—for instance, urban “greening” efforts that generate vegetation to better host ticks and larger wildlife species, unique local eradication efforts, and general public health awareness—to create a complex and often-confounding picture.
LaDeau says that the geographic pattern of vector-borne disease in the region is shifting. “The Northeast hasn’t had a lot of vector-borne epidemics, and Lyme and the tick-borne ones haven’t really moved into the cities yet,” she says. “There are lots of data and reasons to suspect that that is going to change.”
Like other human health problems, including COVID-19, the brunt of vector-borne disease may already fall more heavily on poorer communities. “Areas where the landscape is less managed and manicured tend to have more vectors,” LaDeau says. “One of my colleagues published a paper looking at yards across Dutchess County. One of the predictors of tick abundance was the amount of trash in the yard.” This has urban implications, she says, citing an example in Baltimore, where disparities in sanitation practices between neighborhoods where trash is picked up once a week versus twice a week contribute to producing more and larger mosquitoes in poorer neighborhoods. There is also a significant testing gap across the socioeconomic spectrum: wealthier people are more likely to be tested for vector-borne diseases.
At this point, preventing the spread of vector-borne disease remains primarily a matter of personal responsibility. “Most of the interventions [for ticks] are at the backyard level,” says Diuk-Wasser. “We know there are products that you can spray on your yard and they’re quite effective, but that depends on the individual homeowner, and unfortunately these are often synthetic and people don’t want to use them because of environmental or health concerns.” LaDeau puts it simply: “For both tick-borne and mosquito-borne disease, the most effective protection is still self-protection: don’t get bit.”
But the growing threat of future epidemics suggests a need to move beyond individual efforts toward community-level management and awareness. “We have to somehow control the arrival and the establishment [of vectors] early on, before they spread out,” says LaDeau. “It’s going to require community engagement at a level that we have not seen, or been successful with, in any other public health [intervention]. Everybody’s got to get rid of mosquito-breeding habitat, all summer, and be aware.”
One of Diuk-Wasser’s projects gathers information on tick exposure directly from impacted communities. Using an app—The Tick App—her team compiles data submitted on tick exposure incidents from users in order to better understand where tick spread is occurring. Diuk-Wasser’s team is currently working on an article comparing tick exposure in backyards versus public natural spaces, like parks, over the last year.
Likewise, the Cary Institute is now in the midst of The Tick Project, a five-year study testing the efficacy of two separate tick interventions on the neighborhood level: a commercial product called Met52 derived from a tick-killing fungus, and the “Tick Control System,” small traps that attract the small mammals that carry Lyme and kill ticks they host.
For many scientists, the hope is to find new community-level, environmentally friendly interventions that can be deployed at scale. In many cases, efficacy and utility may come down to community members themselves, LeDeau says. “Humans and human behavior and their perceptions are a really hard thing to model, and are probably a stronger driver than climate on its own.”