The media dubbed it The Week That America Called in Sick. It was early January 2022, the first full week after the winter holidays, when most of us return to some form of work. This year, all bets were off because America’s Christmas present was the Omicron variant—a highly contagious yet purportedly milder version of COVID-19. Suddenly, it seemed like everyone we knew was getting it. Nearly two years in, we were jolted back to high alert, yet we found ourselves in completely new pandemic territory. Eager to understand Omicron’s impacts in real time, we reached out to real people in our communities. From young parents to healthcare workers on the frontlines, the stories gathered below paint a picture of a pandemic moment marked by frustration, confusion, exhaustion, and (yes, it dies hard)—hope.
Jump to read stories from:
- The single mom who runs her own ad agency in Beacon
- The direct primary care physician in Newburgh
- Two parents of teenagers in Saugerties
- The COVID-19 nurse in Kingston
- The high school teacher in Onteora
- The college student in Poughkeepsie
- The single mom and town board member in Middletown
- The musician in Woodstock with a gig in NYC
I Want My Village Back
Gracelyn Woods, a single mom who runs a creative ad agency out of her home in Beacon
My daughter, Hazel, was three months old when COVID started. We were always at risk because it was hard to keep our pod small—her father is an FDNY firefighter who lives with 12 other guys. And Hazel’s in daycare. So I was testing her often to keep an eye out for it. Five days after Christmas, she tested positive. She gave it to me a couple of days later.
We had the same mild symptoms, like runny nose. I only felt pretty bad for one night. And to be honest, I don’t know if it was psychosomatic. I’m vaccinated and boosted. We’ve just been trying to scurry through.
After 10 days, it’s getting really Lord of the Flies here. She’s bored and it’s cold outside so we can’t go out much. She’s used to spending most days with 10 other kids. She’s a social child, so she’s becoming very dysregulated. It’s confusing. Why are we locked in the house? Where are my friends? Why is Mommy crying?
The whole “it takes a village” thing would be great, but it really doesn’t apply during COVID. Everybody is trying to protect their own village, so you can’t really ask for all the help that you need because you’re trying to keep everybody safe. My mom is nearby, but during this time of isolation, I don’t want to expose her. It’s hard. I can’t work when Hazel’s drawing on the walls. I’m a business owner and my business survives on me being engaged.
I’m disheartened by the new CDC guidelines because I feel like it’s misinformation. They lowered the isolation period to five days, but the reality is different. At five days, I took Hazel to her pediatrician and she was still testing positive. They said it’s likely that she’s going to test positive for the full 10 days. The five-day thing is hopeful, but it’s not realistic.
I’d love to see our communities do a little bit more, because I know some families that are struggling right now. My friends and I are fortunate to be able to get food deliveries and be in a good financial position, but I worry about the people who don’t have those options. If you can’t get out of the house to the soup kitchen or wherever, who’s helping you?
My Colleagues Are Tired
Catherine Agricola, MD, a direct primary care physician in Newburgh
A few times during the pandemic, there have been stretches of time where you end up reaching a stride or a rhythm. A workflow for testing and managing and tracking. Guidelines that haven’t changed in weeks. A respite from the pendulum swings.
Then you see the Omicron wave offshore and brace for impact. It’s back to swirling new information, updated policies, unsynchronized change.
The disruptive distress has been pervasive. A patient set to start a new job only to test positive and be out for another 10 days. People with symptoms that couldn’t find test appointments for a week. The yearning to be with others. The fear of seeing anyone.
I haven’t been able to manage patients with COVID the way I did before. It isn’t feasible. The volume is too high. And the outpatient treatments that were available are now ineffective. Newer treatments are scarce.
I have started to see patients get through COVID differently. They haven’t sounded as sick over the phone. They weren’t laid up in bed. There were one or two bad days instead of seven. One patient expressed relief that her test was positive after the onset of relatively mild symptoms. The looming fear she’d had for so long was lifted. And she was okay.
I have felt a small hope that Omicron may be an epidemiologic endgame of sorts. If it really is milder and we have a mostly vaccinated society, we might get more community immunity with less tragedy. It’s just, can the system handle this last big push? I’m tired. My colleagues are tired. The system is strained. Even if a smaller percentage of infected patients gets really sick, a small percentage of a large number is still a lot of sick people.
I’m holding out hope that we will get over this surge and maybe transition from a pandemic to an epidemic. Maybe with an epilogue on the horizon. I don’t know. But I’m keeping reasonable hope.
Blindsided
Jason and Sheila, parents of two teens in Saugerties
Jason: Everyone I knew said they had a cold [in late December]. They all tested negative for COVID. So, when I got what I thought was a cold and tested negative on a home test, my initial reaction was to shrug it off. It wasn’t until a couple of days later that I heard everyone was testing negative first. For us, it meant, Oh, crap. I had this horrible guilt that I likely brought it into the family. All four of us got it. I think I got it through my eyes from someone blowing a vape. It was the only thing I could think of when I tried to retrace my steps.
The frustration was that we’ve been so careful, for so long. Always wearing masks, washing our hands, hand sanitizer everywhere, double masking when appropriate. We’re double vaxxed and boosted. I guess I got a mild case because of that. But it’s still shocking, the misunderstanding of what “highly infectious” means, compared to the previous guidelines. There just wasn’t a lot of information. I felt blindsided. You become sort of skeptical about the guidance in general, which is a bummer.
I don’t feel so scared about being sick, but that doesn’t mean it’s any less impactful.
Sheila in SaugertiesSheila: We had a lot of sneezing, bad headache for a couple of days, and then just lethargy. Everything was exhausting. Our 18-year-old had it the worst, because she got her booster on the same day that she was exhibiting her first symptoms of COVID. She was throwing up all night. It was just awful. We found out that if you happen to be unlucky enough to get your booster while contracting the virus, you will get pounded. The rest of us had really mild symptoms. Just long-lasting.
For me, I go back and forth: In some ways I feel kind of happy that I got it because maybe it helps my immune system, and maybe I helped the greater herd immunity. But that doesn’t make it less intense of a virus, because the hospital systems are still taxed, people are still having to close schools and jobs, and there’s not enough work staff to keep the country running in a way where everybody’s taken care of. I don’t feel so scared about being sick, but that doesn’t mean it’s any less impactful.
Exhausted and Bitter
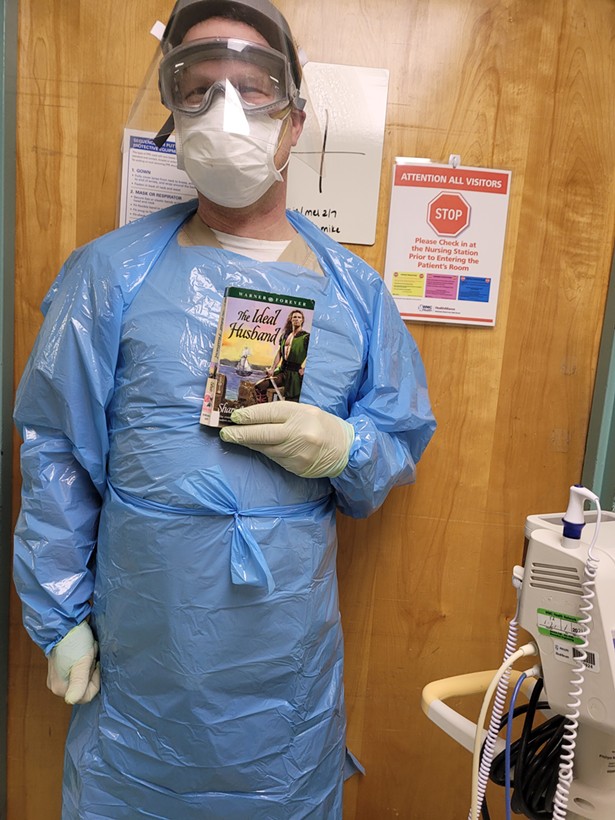
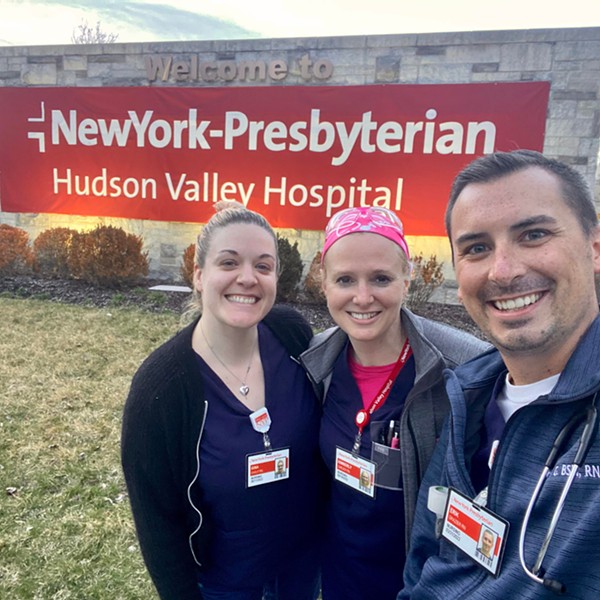
Lawrence Clayton, an RN at HealthAlliance Hospital: Broadway Campus
Yesterday on my unit, 20 of 25 beds were positive. One of my colleagues started feeling ill but wasn’t allowed to leave work. This morning she tested positive (she’s fully vaccinated). I don’t believe I was around her unmasked, but because we are so overwhelmed and understaffed, meal breaks are super-rushed five-minute affairs where you duck into the break room and shovel food down your throat. (A half-hour’s pay is deducted for the meal break nonetheless.) The unspoken understanding is that COVID does not exist in the break room.
A few weeks ago, I had a patient dying of COVID. Her loved one asked if he could visit, even though he was unvaccinated. I had to tell him no—per hospital policy, all visitors must be vaccinated or have a recent negative test. I wanted to scream into the phone, “Just get the shot, you moron!” Of course, I didn’t. I think I have some PTSD. We get screamed at by patients and families on a daily basis. I’ve been accused of medical kidnapping and neglect.
We are so very short-staffed. On a typical day, I have six or seven patients, sometimes eight. Five is the maximum number a nurse can truly be responsible for. Worse, we’re desperately short on nurse aides. We often have zero or one for the whole 25-bed unit. Without that support, we’re unable to care for our patients properly. Call bells go unanswered, vital signs aren’t taken, people end up lying in their own excrement as we triage needs.
You always stop and ask another nurse if she’s okay, even if you’re drowning, because if we don’t have each other’s back, we don’t have anything. I can take two seconds and help pull up a patient in bed, pull medicine if my colleague is “dirty” (wearing contaminated PPE), or hand her a pitcher of ice water or a saline flush.
WMC fired over 40 nurses and technicians last summer. Since then, many more have quit. New people have been hired, but not enough to stem the flow of departures. I get multiple calls and texts each day from traveling nurse agencies promising big bucks to go elsewhere. Why do I stay? I have a young child here. I feel a responsibility to my colleagues and my community. But it feels unsustainable.
Two years into this pandemic, I am so very exhausted and so incredibly bitter. Get vaccinated. Wear a mask. That’s all I’ve got.
Cultivating Gentleness
Alicia Curlew, a social studies teacher at Onteora High School for 21 years
The nervousness has come back, and it’s brought renewed focus on enforcing social distancing guidelines. That’s tough because it puts teachers in the position of being disciplinarians and distracts from learning. A lot of our kids are vaccinated, so I try to remind myself that they’re less likely to get sick. And our administration at Onteora has been really great and responsible.
You’re balancing two things: You don’t want anybody to get sick, but you also don’t want them to get quarantined because they were sitting too close together. I teach mostly older kids, and at that point some of it is in their hands. Some have a higher risk of getting more sick, and some live with vulnerable family members.
It’s been exhausting and stressful. It’s caused me to think a lot about what I do and how I do it. For me, having a good relationship with the students is really important. If they’re not feeling safe and comfortable, they’re not going to learn. But the way to make kids feel safe has changed—now it’s not just about being comfortable in a high school environment, which most of us wouldn’t go back to in the first place. Then you bring in school shootings, and now this health crisis.
Recognizing how vulnerable teenagers are is at the forefront of my mind all the time now. We’ve had to become very flexible and it requires a lot of gentleness. I have coped by talking with my friends and colleagues a lot more deeply over the past couple of years. It’s not just about ideas for the classroom, but the “what are we doing?” kinds of questions. And I’ve made a conscious effort to take time for myself, even if it’s just locking myself in the bedroom for 20 minutes when I get home from work before I interact with my own family.
At the beginning of the pandemic, it was “teachers are awesome!” but it quickly devolved into “teachers don’t want to work.” It’s very disheartening to hear things like that. People have to understand how difficult and unsatisfying it is to teach remotely. When teachers arrive at that position, it’s because they’re seeing that things are not really okay. They want what is best for the students. I don’t want to be the one making a decision about whether the school is fully open or remote, but I do think teachers have a certain understanding of what’s happening and should be heard when they have concerns.
Far From Home
Diego Scala Chavez, a Vassar College neuroscience major, class of ‘22, from Monterrey, Mexico
I don’t feel that great today, so I’m getting a PCR result, hopefully very soon. I’m keeping myself optimistic and just hoping for the best.
When I went on spring break [in 2020], I thought I was going to have a pleasant vacation. I went to Los Angeles and stayed with one of my friends, and we got the call there: This wasn’t going away. This is serious.
I had to come back, because I couldn’t fly home. That April I was basically stuck without even being able to access a dormitory. I had to find some place to stay until the summer.
I think those were some of the worst months of my life. I felt so detached from everybody else. One of my friends, who was also an international student from Bangladesh, offered me a place to stay in his home, to live off campus. But all of my clothing, all of my stuff, my books, was in my dormitory. I didn’t have access to them. I was scared to go to the supermarket and I didn’t really have secure food options. I would buy a box of pasta and chicken and try to ration it out for a while. All of this while still doing classes but not being really able at all to focus on them.
I flew back home over the summer and immediately tested positive. I had two Pfizer vaccines already. And I had horrible symptoms. I felt like my whole body was in pain, like if I just ran a marathon. I only get to see my family once or twice a year. And to come back after so long, after so much time not seeing them, and just wanting to see my grandma and see my friends and everybody, I had to spend two weeks isolated and doing nothing by myself.
As college students, where a lot of your life revolves around interactions and meeting new people and experiencing these things, so much of that was taken away. It’s hard. There’s this cultural shift towards this sense of unease and collective anxiety.
I owe so much of my sanity to my friends and family. Especially my friends. My friends really just feel like a family to me when I’m away from home. I think we have allowed ourselves to be much more emotionally vulnerable with each other, and I feel like we’ve grown a lot together. I’ve also felt I need to make the most out of what we can do. Start new projects, do new things, gatherings with friends when it’s allowed. Practice your new hobbies. Things that I really took for granted at the beginning.
I’ve crossed every single finger and knocked on every piece of wood. I’m just really hoping that my travel plans aren’t affected by this result.
Balancing Act
Robin Williams, a health insurance agent, mom to 11-year-old River and 9-year-old Owen, and newly elected town board member in the Delaware County town of Middletown
Well, I just had it. Thankfully, I was triple vaxxed going into it. I think that helped. My kids were at one vaccine, and it pretty much was just a really inconvenient cold.
My son tested positive January 1st. I emailed [the town board] January 2nd—the meeting was the 5th—and I said, “My son tested positive. I have to quarantine. I’m sure this has been a balancing act for the past two years for the board. Can I ask someone to have a Zoom open for me so I can attend virtually, or maybe via phone?” Nobody responded.
That was something that I had actually requested before the pandemic even started, because I’m a single mom, and there were nights where I couldn’t leave my then-six- or seven-year-old home. I just wanted to be able to tune in. If the technology is there, I don't understand why we’re not trying to make it fit.
It was a perfect representation of the past two years for me. I finally got COVID. I’ve avoided it this whole time. I’m a newly elected official, going, okay, what can I do? And it was just crickets. We’re two years in, with all of the capabilities and adjustments we’ve made during this pandemic—and you still don’t have a way to do what you were just elected to do.
I know it seems bizarre to be spread so thin as a mom, and the single income in my household, to be involved with lots of different things and then to want to run for a local government position. But it’s [people like me] who see what’s really going on in the community. We hear what people want and need. I feel like I’m in touch with our town.
We’re two years in, with all of the capabilities and adjustments we’ve made—and you still don’t have a way to do what you were just elected to do.
Robin WilliamsI’m trying to be careful as I talk to people about my experience of being sick. I’m pretty healthy, I was boosted, I was able to isolate. We’re only as strong as our weakest links. People who are immunocompromised, or who can’t afford to upgrade their mask quality because they’re expensive—like, somebody gave me a box of N95s for Christmas. That’s where we’re at.
Spooked and Surreal
David G., a musician in Woodstock
My wife got sick first, and a few days later I felt something in my throat, but we both tested negative initially on a home test on different days. So I went to the city for a gig and tried to be extra careful. They had already made it a private show because Omicron was hitting New York, and very few people showed up.
The next day my throat was still sore and the body aches started up. Home tests were becoming impossible to get, but we had friends coming from Italy, and I asked them to bring as many kits as possible. They dropped one off, and I tested positive. My wife saw her doctor, and she tested positive too.
She slept it off in two to three days, but all of Christmas weekend I had a headache and body aches and could not sleep. Early one morning, I got up to go to the bathroom and felt really dizzy. I couldn’t see—there was this gray wash over everything—and then I passed out. When my wife found me sprawled on the toilet, my clothes were drenched and my hands had this tingling sensation. She brought me coconut water and a banana and made me some miso soup. Passing out scared me, but the idea of going to the hospital scared me too, so we didn’t. I think it was mainly dehydration. After that, I was okay. My low fever passed and I could finally sleep.
I lived to tell the tale, but there’s such a stigma to it. When you’ve never had COVID, you say, “I’ve managed to avoid this” with a sense of pride or something. Then you get it and you’re downplaying it: “Oh, it’s no big deal.” But I was definitely spooked. My brother got it before the vaccine rollout, and he was out for weeks. He basically has long COVID now.
By New Year’s Eve, I was testing negative, so we went to a friend’s place in the city. We got an Uber in like three minutes and it was normal, everyday pricing. I was like, Wait, what? There’s usually an hour-and-a-half wait and it’s 10 times the price. But the city was a ghost town on New Year’s. It was so surreal.
This article was also published in the February 2022 issue of Chronogram.