In the past few decades, the opioid epidemic has plagued the nation, with a 200 percent increase in opioid-related deaths since 2000. The Hudson Valley and Catskills are no exception. Members of our community have stood by watching with helplessness as these drugs strip the life and humanity from innocent people.
For the past few years, Sullivan County has been the county with the highest rate of opioid overdose deaths in New York State, with 39.8 people per 100,000 dying from opioids in 2019, the most recent year of available data. (Early evidence suggests the epidemic has only worsened during the pandemic.) Dutchess, Orange, and Ulster counties were also in the top nine for age-adjusted opioid overdose deaths per 100,000 in 2019.
Despite these rates, doctors are still largely prescribing opioids, even in communities where overdose and death rates are high and increasing. Most opioids are produced by large pharmaceutical companies and prescribed as painkillers. Abuse of prescription opioids is unique in that users are not getting their drugs from the “streets”—they’re getting them from either a licensed medical professional or from someone else with a prescription from a licensed medical professional.
It’s hard not to feel helpless in the struggle against addiction and overdose, but there are ways to help. The most immediate way to make a difference is through harm reduction. Harm reduction entails reducing the negative consequences associated with using drugs. Being educated on opioids and their effects, and knowing the signs of an overdose and what to do in the event of one are ways to practice harm reduction.
What Are Opioids?
Opioids act on the body’s central nervous system, the brain and spinal cord. They attach to and activate opioid receptor proteins (located mostly in the central nervous system), and prevent pain signals from reaching the brain. This is why some opioids are medically prescribed to patients with chronic illnesses and to patients with painful injuries.
The brain is the control center for all of our body’s processes, including breathing, sleeping, and digestion. Opioids depress, or slow down, certain functions of the brain, particularly respiration, as opioid receptors are abundantly located in parts of the brain that control breathing. Opioids can also cause drowsiness, constipation, and nausea.
“Opioids” is an umbrella term for natural, synthetic, and semisynthetic opioids. “Opiates” refer only to natural opioids, such as heroin, codeine, and morphine. These terms are often used interchangeably by the media and general public. Other opioids include fentanyl, methadone, oxycodone, hydrocodone, tramadol, and less commonly, hydromorphone and oxymorphone. Percocet, Vicodin, and OxyContin are brand names for different opioids. Heroin is the most common illicit opioid; the others are legally prescribed. Of course, there is a black market for everything and users can purchase prescription opioids illegally.
Fentanyl, a synthetic opioid, has been prominent in the news in the past few years, as it has been linked to many accidental overdoses and deaths. Fentanyl is increasingly being added to other street drugs, like cocaine or methamphetamine, because it’s extremely potent. This makes drugs more powerful, cheaper, and more addictive. As a result, one-time drug users and young adults doing “party drugs” are at a high risk for overdose. Additionally, mixing opioids with alcohol or other drugs makes overdosing more likely.
Opioid Myths
The rise in fentanyl has corresponded with an increase in horror stories about the dangers of indirect opioid ingestion. Law enforcement officers have shared anecdotes about accidentally coming into contact with powdered fentanyl, or touching someone who had overdosed, and then experiencing an overdose themselves.
These claims are false. In their powdered form, fentanyl and other opioids cannot be absorbed through the skin. (This is possible in liquid form, but opioids are usually found in powdered or pill form.) One can come into contact with fentanyl through a needle stick, inhalation, or if it comes in direct contact with the mucous membranes that line your eyes, nose, and mouth. You cannot ingest it by providing CPR or rescue breathing to someone who has overdosed.
Oftentimes, when someone is overdosing, bystanders are afraid to get help. This is out of fear of getting that person in trouble, or of getting in trouble themselves. New York State’s Good Samaritan Law ensures that you and the person overdosing will be legally protected if you call 911 in the event of an overdose. If you are underage, if you also took drugs, and/or if you are still in possession of drugs, you won’t get in legal trouble for getting help.
How to Help Someone Who Is Overdosing
In order to help someone who is overdosing on opioids, one must first know the signs. Since opioids depress the central nervous system, one of the key signs of an overdose is slow or shallow breathing, or no breathing at all. Other signs of an overdose include disorientation; sleepiness; difficulty speaking; unconsciousness; pale, blue, or grayish skin, particularly near the fingertips, mouth, and face; and tiny pupils.
Once you have recognized that an overdose is taking place, call 911 immediately.
If the person is conscious, try to keep them awake. If they are unconscious, try to wake them up by tapping, shaking, and yelling at them. If they are still unresponsive, press your knuckles into their breastbone, squeeze their earlobes, or pinch them.
If you have Naloxone or another opioid antagonist, administer it. The one most commonly available is Narcan nasal spray. Each dose of Narcan contains 4mg of medicine. Insert the tip into one nostril until your two fingers are flush against either side of the nostril, and push the piece in the middle, releasing the entire contents into one nostril.
Roll the person on their side with their arm and leg over their body—the recovery position.
The medicine will take a few minutes to work, and if the person regains consciousness, expect them to be agitated and possibly aggressive. If they do not regain consciousness after several minutes, you can administer another 4mg nasal spray.
If you do not have Naloxone or another opioid antagonist on hand, determine if the person is breathing. If they are, put them in the recovery position while calling 911. If they are not breathing, call 911 and then begin CPR.
CPR on adults consists of a 30:2 compression to rescue breath ratio. This means that you begin CPR with 30 chest compressions, followed by two rescue breaths, and then repeat. Pinch the person’s nose and create a seal with your fingers around their mouth for rescue breathing. Do this for as long as you can until EMS arrives or until the person regains consciousness. If there is anyone else around who is capable of performing CPR, alternate with them.
If you have administered Naloxone and the person has regained consciousness, you should still call 911 if you haven’t already. It is possible for that person to overdose again later on.
Laws and Legislation
In October of 2021, Governor Kathy Hochul signed several laws intended to fight opioid overdose. One decriminalizes drug-related paraphernalia, including the sale and possession of hypodermic needles and syringes. Another broadens the opportunities for someone struggling with substance use to be sentenced to a treatment facility instead of being given jail time.
Perhaps most relevant to bystanders who want to help, two of the laws should widen the use of opioid antagonists, which work by attaching to opioid receptors, thus preventing the opioid itself from attaching and activating those receptors. Naloxone, more commonly known by its brand name of Narcan, is an example of an opioid antagonist. Carrying an opioid antagonist without a prescription has been grounds for a criminal charge in the past, but the new law decriminalizes possession of opioid antagonists. The other established an online directory for distributors of opioid antagonists, making them more accessible.
On March 31, Hochul also granted $1.6 million to eight different addiction service providers in the state, which will allow them to establish “mobile medication units.” These mobile units will aid in providing addiction resources, including dispensing drugs such as methadone, to those trying to overcome opioid substance use. This is aimed at providing the resources to those who need help but may not have access to the opportunities needed to get it.
A bill signed in December of 2021 removes the prior authorization mandate in New York’s Medicaid program on certain medications used to treat opioid addiction. These include buprenorphine and methadone, and the opioid antagonist Naltrexone, which works in the same way as Naloxone. This law will enable people with Medicaid to access these medications without delay.
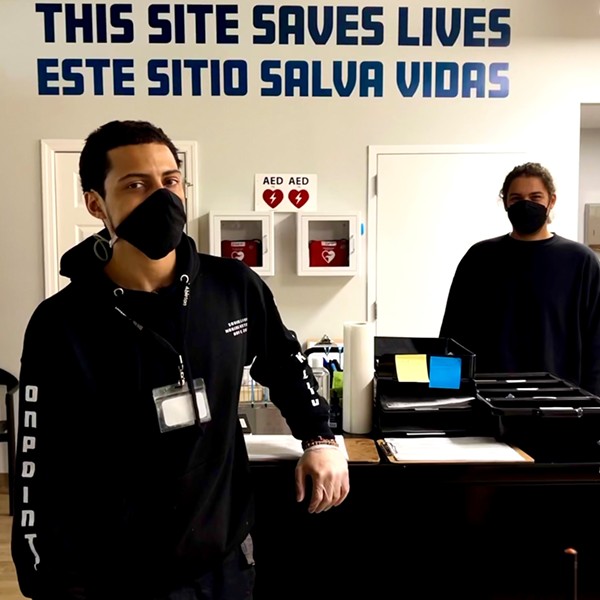
There has also been more of a national effort to promote harm reduction in the opioid epidemic. There has been a push in several cities throughout the country, including New York City, to implement safe consumption services, or supervised injection sites. Safe consumption services are places where individuals can use drugs in a safe and controlled environment. The benefits of this include decreased overdose rates, decreased transmission of diseases, and proper disposal of drug paraphernalia. Counseling, health, and treatment resources are also provided at these facilities.
Resources
There are many resources available for people who use drugs or those who know people that do. These links are just a handful that offer addiction support services, Naloxone training, and information on how to get free Naloxone.
- The National Harm Reduction Coalition website lists locations across New York State (and throughout the country) that offer free Naloxone and training.
- NEXTDistro offers free virtual Naloxone and training in English and Spanish, among other resources.
- There are organizations that offer free in-person Narcan and harm reduction services in the Hudson Valley. One of these organizations, Ulster County Outreach Program, has pop-ups on college campuses where they train students in harm reduction and Narcan use. They provide free Narcan upon training in addition to many other resources.
- Many pharmacies including certain Walgreens, CVS, Rite Aid, and Duane Reade locations sell Naloxone. Some insurances cover the cost. You can find participating pharmacies at the NYS DOH pharmacy directory.
- The NYS DOH opioid overdose prevention program directory lists opioid overdose prevention and addiction resources based on zip code.
- This website lists crisis and suicide hotlines and websites in New York State by county (and national ones).
More is being done through New York State law to combat the opioid epidemic, but the greatest way to be an active part of change is to educate oneself, be prepared, and share these resources with others. Addiction is a tragic illness with many root causes, but overdose death is preventable.